

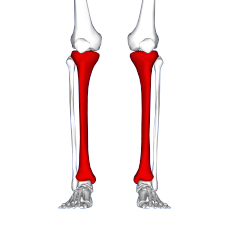
Red area represents tibia. MTSS pain found on inner and lower 2/3rds of tibia.
|
Shin splints are the most prevalent lower leg injury and affect a broad range of individuals. It affects mostly runners and accounts for approximately 13% to 17% of all running-related injuries. High school age runners see shin splints injury rates of approximately 13%. Aerobic dancers have also been known to suffer from shin splints, with injury rates as high as 22%. Military personnel undergoing basic training experience shin splints injury rates between 4%-6.4% and 7.9%.
Top of page
Signs and symptoms
Shin splint pain is described as a recurring dull ache along the inner part of the lower two-thirds of the tibia. In contrast, stress fracture pain is localized to the fracture site.
Biomechanically, over-pronation is the common cause for shin splints and action should be taken to offset the biomechanical irregularity. Pronation occurs when the ankle bonemoves downward and towards the middle to create a more stable point of contact with the ground. In other words, the ankle rolls inwards so that more of the arch has contact with the ground. This abnormal movement causes muscles to fatigue more quickly and to be unable to absorb any shock from the foot hitting the ground.
Top of page
Causes
While the exact cause is unknown, shin splints can be attributed to the overloading of the lower leg due to biomechanical irregularities resulting in an increase in stress exerted on the tibia. A sudden increase in intensity or frequency in activity level fatigues muscles too quickly to properly help absorb shock, forcing the tibia to absorb most of that shock. This stress is associated with the onset of shin splints. Muscle imbalance, including weak core muscles, inflexibility and tightness of lower leg muscles, including the gastrocnemius,soleus, and plantar muscles (commonly the flexor digitorum longus) can increase the possibility of shin splints.
The pain associated with shin splints is caused from a disruption of Sharpey's fibres that connect the medial soleus fascia through the periosteum of the tibia where it inserts into the bone. With repetitive stress, the impact forces eccentrically fatigue the soleus and create repeated tibial bending or bowing, contributing to shin splints. The impact is made worse by running uphill, downhill, on uneven terrain, or on hard surfaces. Improper footwear, including worn-out shoes, can also contribute to shin splints.
Top of page
Diagnosis
Shin splints can be diagnosed by a physician after taking a thorough history and performing a complete physical examination. The physical examination focuses on palpable, or gentle pressure, tenderness over a 4–6 inch section on the lower, inside shin area. The pain has been described as a dull ache to an intense pain that increases during exercise, and some individuals experience swelling in the pain area. Clinical history focuses on an individual's previous history with shin splints. People who have previously had shin splints are more likely to have it again.
Vascular and neurological examinations produce normal results in patients with shin splints. Radiographies and three-phase bone scans are recommended to differentiate between shin splints and other causes of chronic leg pain. Bone sctintigraphy and MRI scans can be used to differentiate between stress fractures and shin splints.
It is important to differentiate between different lower leg pain injuries, including shin splints, stress fractures, compartment syndrome, nerve entrapment, and popliteal artery entrapment syndrome. These conditions often have many overlapping symptoms which makes a final diagnosis difficult, and correct diagnosis is needed to determine the most appropriate treatment.
Top of page
Treatment
Typical treatments include rest, ice, strengthen and gradually returning to activity. Rest and ice work to allow the tibia to recover from sudden, high levels of stress and reduce inflammation and pain levels. It is important to significantly reduce any pain or swelling before returning to activity. Strengthening exercises should be performed after pain has subsided, focusing on lower leg and hip muscles. Individuals should gradually return to activity, beginning with a short and low intensity level. Over multiple weeks, they can slowly work up to normal activity level. It is important to decrease activity level if any pain returns. Individuals should consider running on other surfaces besides asphalt, such as grass, to decrease the amount of force the lower leg must absorb. Orthoses and insoles help to offset biomechanical irregularities, like pronation, and help to support the arch of the foot.
Less common forms of treatment for more severe cases of shin splints include extracorporeal shockwave therapy (ESWT) and surgery. Surgery is only performed in extreme cases where more conservative options have been tried for at least a year. However, surgery does not guarantee 100% recovery.
Top of page
Risk factors
Risk factors for developing shin splints include:
- Excessive pronation at subtalar joint
- Excessively tight calf muscles (which can cause excessive pronation)
- Engaging the medial shin muscle in excessive amounts of eccentric muscle activity
- Undertaking high-impact exercises on hard, noncompliant surfaces (ex: running on asphalt or concrete)
- Smoking and low fitness level
While medial tibial stress syndrome is the most common form of shin splints, compartment syndrome and stress fractures are also common forms of shin splints. Females are 1.5 to 3.5 times more likely to progress to stress fractures from shin splints. This is due in part to females having a higher incidence of diminished bone density and osteoporosis.
Back to top
|
Page Content |


