

The tendons of the rotator cuff, not the muscles, are most commonly involved, and of the four, the supraspinatus is most frequently affected, as it passes below the acromion. Such a tear usually occurs at its point of insertion onto the humeral head at the greater tubercle.
| Rotator cuff tear | |
|---|---|
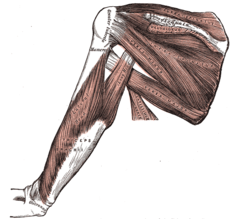
Muscles on the dorsum of the scapula, and the triceps brachii
|
The cuff is responsible for stabilizing the glenohumeral joint, abducting, externally rotating, and internally rotating the humerus. When shoulder trauma occurs, these functions can be compromised. Because individuals are highly dependent on the shoulder for many activities, overuse of the muscles can lead to tears, the vast majority again occurring in the supraspinatus tendon.
Top of page
Signs and symptoms
Many rotator cuff tears are asymptomatic. They are known to increase in frequency with age and the most common cause is age-related degeneration and, less frequently,sports injuries or trauma. Both partial and full thickness tears have been found on post mortem and MRI studies in those without any history of shoulder pain or symptoms. However, the most common presentation is shoulder pain or discomfort. This may occur with activity, particularly shoulder activity above the horizontal position, but may also be present at rest in bed. Pain-restricted movement above the horizontal position may be present, as well as weakness with shoulder flexion and abduction.
Top of page
Mechanisms of injury
The two main causes are injury (acute) and degeneration (chronic and cumulative), and the mechanisms involved can be either extrinsicor intrinsic or, probably most commonly, a combination of both.
Acute tears
The amount of stress needed to tear a rotator cuff tendon acutely will depend on the underlying condition of the tendon prior to the stress. In the case of a healthy tendon, the stress needed will be high, such as a fall on the outstretched arm. This stress may occur coincidentally with other injuries such as a dislocation of the shoulder, or separation of the acromioclavicular joint. In the case of a tendon with pre-existing degeneration, the force may be surprisingly modest, such as a sudden lift, particularly with the arm above the horizontal position. This is a common occurrence with rear seated passengers in a motor vehicle collision, regardless of speed.
Chronic tears
Chronic tears are indicative of extended use in conjunction with other factors such as poor biomechanics or muscular imbalance. Ultimately, most are the result of wear that occurs slowly over time as a natural part of aging. They are more common in the dominant arm, but a tear in one shoulder signals an increased risk of a tear in the opposing shoulder. Several factors contribute to degenerative, or chronic, rotator cuff tears of which repetitive stress is the most significant. This stress consists of repeating the same shoulder motions frequently, such as overhead throwing, rowing, and weightlifting. Many jobs that require frequent shoulder movement such as lifting and overhead movements also contribute.
Another factor in older populations is impairment of blood supply. With age, circulation to the rotator cuff tendons decreases, impairing natural ability to repair, ultimately leading to, or contributing to, tears.
The final common factor is impingement syndrome, the most common nonsports-related injury and which occurs when the tendons of the rotator cuff muscles become irritated and inflamed while passing through the subacromial space beneath the acromion. This relatively small space becomes even smaller when the arm is raised in a forward or upward position. Repetitive impingement can inflame the tendons and bursa, resulting in the syndrome.
Extrinsic factors
Well-documented anatomical factors include the morphologic characteristics of the acromion. Hooked, curved, and laterally sloping acromia are strongly associated with cuff tears and may cause tractional damage to the tendon. Conversely, flat acromia may have an insignificant involvement in cuff disease and consequently may be best treated conservatively. The development of these different acromial shapes is likely both genetic and acquired. In the latter case, only age has been positively correlated with progression from flat to curved or hooked. The nature of mechanical activities, such as sports involving the shoulder, along with frequency and intensity of such sports, may be responsible for the adverse development. Sports such as bowling in cricket, swimming, tennis, baseball, and kayaking, are most frequently implicated. However, a progression to a hooked acromion may simply be an adaptation to an already damaged, poorly balanced rotator cuff that is creating increasing stress on the coracoacromial arch. Other anatomical factors that may have significance include os acromiale and acromial spurs. Environmental factors implicated include increasing age, shoulder overuse, smoking, and any medical condition that impairs the inflammatory and healing response, such as diabetes mellitus.
Intrinsic factors
Intrinsic factors refer to injury mechanisms that occur within the rotator cuff itself. The principal is a degenerative-microtrauma model, which supposes that age-related tendon damage compounded by chronic microtrauma results in partial tendon tears that then develop into full rotator cuff tears. As a result of repetitive microtrauma in the setting of a degenerative rotator cuff tendon, inflammatory mediators alter the local environment, and oxidative stress induces tenocyte apoptosis causing further rotator cuff tendon degeneration. A neural theory also exists that suggests neural overstimulation leads to the recruitment of inflammatory cells and may also contribute to tendon degeneration.
Top of page
Pathophysiology

The shoulder is a complex mechanism involving bones, ligaments, joints, muscles, and tendons.
Classification


Tears of the rotator cuff tendon are described as partial or full thickness, and full thickness with complete detachment of the tendons from bone.
- Partial-thickness tears often appear as fraying of an intact tendon.
- Full-thickness tears are "through-and-through". These tears can be small pinpoint, larger buttonhole, or involve the majority of the tendon where it still remains substantially attached to the humeral head and thus maintains function.
- Full-thickness tears may also involve complete detachment of the tendon(s) from the humeral head and may result in significantly impaired shoulder motion and function.
Shoulder pain is variable and may not be proportional to the size of the tear.
Top of page
Diagnosis

Diagnostic modalities, dependent on circumstances, include:
- X-ray
- MRI
- MR arthrography
- Double-contrast arthrography
- Ultrasound.
Clinical judgement, rather than over reliance on MRI or any other modality, is strongly advised in determining the cause of shoulder pain, or planning its treatment, since rotator cuff tears are also found in some without pain or symptoms. The role of X-ray, MRI, and ultrasound, is adjunctive to clinical assessment and serves to confirm a diagnosis provisionally made by a thorough history and physical examination. Over-reliance on imaging may potentially lead to overtreatment or distraction from the true underlying problem.
Symptoms
Symptoms may occur immediately after trauma (acute) or develop over time (chronic).
Acute injury is less frequent than chronic disease, but may follow bouts of forcefully raising the arm against resistance, as occurs in weightlifting, for example. In addition, falling forcefully on the shoulder can cause acute symptoms. Chronic tears occur among individuals who constantly participate in overhead activities, such as pitching or swimming, but can also develop from shoulder tendinitis or rotator cuff disease. Symptoms arising from chronic tears include sporadic worsening of pain, debilitation, and atrophy of the muscles, noticeable pain during rest, crackling sensations (crepitus) when moving the shoulder, and inability to move or lift the arm sufficiently, especially during abduction and flexion motions.
In-office testing
As part of clinical decision-making, a simple, minimally invasive, in-office procedure may be performed, the rotator cuff impingement test. A small amount of a local anesthetic and an injectable corticosteroid are injected into the subacromial space to block pain and to provide anti-inflammatory relief. If pain disappears and shoulder function remains good, no further testing is pursued. The test helps to confirm that the pain arises from the shoulder primarily rather than referred from the neck, heart, or gut.
If pain is relieved, the test is considered positive for rotator-cuff impingement, of which tendinitis and bursitis are major causes. However, partial rotator-cuff tears may also demonstrate good pain relief, so a positive response cannot rule out a partial rotator-cuff tear. However, with demonstration of good, pain-free function, treatment will not change, so the test is useful in helping to avoid overtesting or unnecessary surgery.
Top of page
Prevention
Long-term overuse/abuse of the shoulder joint is generally thought to limit range of motion and productivity due to daily wear and tear of the muscles, and many public web sites offer preventive advice. (See external links) The recommendations usually include:
- regular shoulder exercises to maintain strength and flexibility
- using proper form when lifting or moving heavy weights
- resting the shoulder when experiencing pain
- application of cold packs and heat pads to a painful, inflamed shoulder
- strengthening program to include the back and shoulder girdle muscles as well as the chest, shoulder and upper arm
- adequate rest periods in occupations that require repetitive lifting and reaching
Top of page
Treatment

Those suspected of having a rotator cuff tear are potentially candidates for either operative or non-operative treatment. However, any individual may move from one group to the other based on clinical response and findings on repeated examination.
No evidence of benefit is seen from early rather than delayed surgery, and many with partial tears and some with complete tears will respond to nonoperative management. Consequently, many recommend initial, nonsurgical management. However, early surgical treatment may be considered in significant (>1 cm-1.5 cm) acute tears or in young patients with full-thickness tears who have a significant risk for the development of irreparable rotator cuff changes.
Non-operative treatment

Those with pain but reasonably maintained function are suitable for nonoperative management. This includes oral medications that provide pain relief such as anti-inflammatory agents, topical pain relievers such as cold packs, and if warranted, subacromial corticosteroid/local anesthetic injection. An alternative to injection is iontophoresis, a battery-powered patch which "drives" the medication to the target tissue. A sling may be offered for short-term comfort, with the understanding that undesirable shoulder stiffness can develop with prolonged immobilization. Early physical therapy may afford pain relief with modalities (e.g. iontophoresis) and help to maintain motion. Ultrasound treatment is not efficacious. As pain decreases, strength deficiencies and biomechanical errors can be corrected.
A conservative physical therapy program begins with preliminary rest and restriction from engaging in activities which gave rise to symptoms. Normally, inflammation can usually be controlled within one to two weeks, using a nonsteroidal anti-inflammatory drug and subacromial steroid injections to decrease inflammation, to the point that pain has been significantly decreased to make stretching tolerable. After this short period, rapid stiffening and an increase in pain can result if sufficient stretching has not been implemented.
A gentle, passive range-of-motion program should be started to help prevent stiffness and maintain range of motion during this resting period. Exercises, for the anterior, inferior, and posterior shoulder, should be part of this program. Codman exercises (giant, pudding-stirring), to "permit the patient to abduct the arm by gravity, the supraspinatus remains relaxed, and no fulcrum is required" are widely used. The use of NSAIDs, hot and cold packs, and physical therapy modalities, such as ultrasound, phonophoresis, or iontophoresis, can be instituted during this stretching period, if effective. Corticosteroid injections are recommended two to three months apart with a maximum of three injections. Multiple injections (four or more) have been shown to compromise the results of rotator cuff surgery which result in weakening of the tendon. However, before any rotator cuff strengthening can be started, the shoulder must have a full range of motion.
After a full, painless range of motion is achieved, the patient may advance to a gentle strengthening program.
Several instances occur in which nonoperative treatment would not be suggested:
- 20 to 30-year-old active patient with an acute tear and severe functional deficit from a specific event[38]
- 30 to 50-year-old patient with an acute rotator cuff tear secondary to a specific event[38]
- a highly competitive athlete who is primarily involved in overhead or throwing sports
These patients may need to be treated operatively because rotator cuff repair is necessary for restoration of the normal strength required to return to the preoperative, competitive level of function. Finally, those who do not respond to, or are unsatisfied with, conservative treatment should seek a surgical opinion.
Surgery
The three general surgical approaches are:
- Arthroscopic
- Mini open
- Open-surgical repair.
Even for full-thickness rotator cuff tears, conservative care (i.e., nonsurgical treatment) outcomes are usually reasonably good. However, many patients still suffer disability and pain despite nonsurgical therapies. For massive tears of the rotator cuff, surgery has shown durable outcomes on 10-year follow-up. However, the same study demonstrated ongoing and progressive fatty atrophy and repeat tears of the rotator cuff. MRI evidence of fatty atrophy in the rotator cuff prior to surgery is predicative of a poor surgical outcome. If the rotator cuff is completely torn, surgery is usually required to reattach the tendon to the bone.
If a significant bone spur is present, any of the approaches may include an acromioplasty, a subacromial decompression, as part of the procedure.Subacromial decompression, removal of a small portion of the acromion that overlies the rotator cuff, aims to relieve pressure on the rotator cuff in certain conditions and promote healing and recovery. Although subacromial decompression may be beneficial in the management of partial and full-thickness tear repair, it does not repair the tear itself and arthroscopic decompression has more recently been combined with "mini-open" repair of the rotator cuff, allowing for the repair of the cuff without disruption of the deltoid origin. The results of decompression alone tend to degrade with time, but the combination of repair and decompression appears to be more enduring.
Repair of a complete, full-thickness tear involves tissue suture. The method currently in favor is to place an anchor in the bone at the natural attachment site, with resuture of torn tendon to the anchor. If tissue quality is poor, mesh (collagen, Artelon, or other degradable material) may be used to reinforce the repair. Repair can be performed through an open incision, again requiring detachment of a portion of the deltoid, while a mini-open technique approaches the tear through a deltoid-splitting approach. The latter may cause less injury to muscle and produce better results. Contemporary techniques now use an all arthroscopic approach. Recovery can take as long as three–six months, with a sling being worn for the first one–six weeks.
In a small minority of cases where extensive arthritis has developed, an option is shoulder joint replacement (arthroplasty).
Top of page
Rehabilitation
Rehabilitation after surgery consists of three stages.
- The arm is immobilized so that the muscle can heal.
- When appropriate, a therapist assists with passive exercises to regain range of motion.
- The arm is gradually exercised actively, with a goal of regaining and enhancing strength.
Following arthroscopic rotator-cuff repair surgery, patients undergo rehabilitation to regain shoulder function. Orthopaedic surgeons stress that physical therapy is crucial to healing. Exercises decrease shoulder pain, strengthen the joint, and improve the arm's range of motion. Therapists, in conjunction with the surgeon, design workout regimens in accordance with individuals' needs and risk factors.
Top of page
Epidemiology
Incidence
A rotator cuff tear can be caused by the weakening of the rotator cuff tendons. This weakening can be caused by age or how often the rotator cuff is used. Adults over the age of 60 are more susceptible to a rotator cuff tear. According to a study in the Journal of Orthopaedic Surgery and Traumatology the frequency of rotator cuff tears can increase with age. The study shows the participants that were the ages of 70–90 years old had a rate of rotator cuff tears that were 1 to 5. The participants who were 90+ years old the frequency of a rotator cuff tear jumped to 1 to 3. This study shows that with an increase in age there is also an increase in the probability of a rotator cuff tear.
Prevalence

According to a study in the Journal of Orthopaedics the prevalence of a rotator cuff tear was considerably greater in males than in females within the ages of 50–60 years old, within the ages of 70–80 years old there wasn’t much difference in prevalence. The data of this study showed that the prevalence of a rotator cuff tear in the general population is 22.1%


